Computed Tomography
Technical advances in CT scanning, including the development of multidetector-array scanners, have led to the emergence of CT scanning as an important diagnostic technique in suspected PE.[13, 14] Contrast-enhanced CT scanning is increasingly used as the initial radiologic study in the diagnosis of PE, especially in patients with abnormal chest radiographs in whom scintigraphic results are more likely to be nondiagnostic. (See the image below.)[4, 5, 6]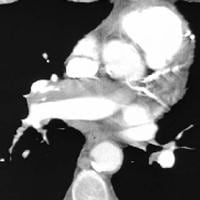 Computed
tomography angiogram in a 69-year-old man with known pulmonary arterial
hypertension and a history of chronic pulmonary embolism. This image
shows an eccentric mural thrombus with punctate calcification along the
anterior wall of the right lower interlobar artery. CT
scanning shows emboli directly, as does pulmonary angiography, and it is
also noninvasive, cheaper, and widely available. CT scanning is the
only test that can provide significant additional information related to
alternate diagnoses; this is a clear advantage of CT scanning compared
with either pulmonary angiography or scintigraphy.[15] A CT image depicting an acute pulmonary embolism is provided below.
Computed
tomography angiogram in a 69-year-old man with known pulmonary arterial
hypertension and a history of chronic pulmonary embolism. This image
shows an eccentric mural thrombus with punctate calcification along the
anterior wall of the right lower interlobar artery. CT
scanning shows emboli directly, as does pulmonary angiography, and it is
also noninvasive, cheaper, and widely available. CT scanning is the
only test that can provide significant additional information related to
alternate diagnoses; this is a clear advantage of CT scanning compared
with either pulmonary angiography or scintigraphy.[15] A CT image depicting an acute pulmonary embolism is provided below.Because DVT and PE are part of the same disease process, CT venography can easily be performed after CT pulmonary angiography, without the administration of additional contrast material.[11, 16, 17] This study requires only a few extra minutes and allows "one-stop imaging" for PE and DVT.
The technique for CT pulmonary angiography with single-section helical CT involves the following parameters: 3-mm collimation, 2-mm reconstruction interval, pitch of 2, and an average acquisition time of 24 seconds. Iodinated contrast medium is administered as a bolus with an automated injector. Generally, a large volume (100-150 mL) of contrast material is administered at a high flow rate (4 mL/s) for good-quality diagnostic opacification of vessels.[18]
CT venograms can be acquired 3-4 minutes after the start of the administration of contrast material. The new multidetector-row CT (MDCT) scanners are considerably faster, allowing the performance of thin-section (1.25-mm) helical CT pulmonary angiography during a shorter breath hold (15-17 seconds). With introduction of dual-source CT technology, ECG-gated CTA of the chest may become practical and help provide clinicians with cardiac functional information.
Efforts should be made to minimize the radiation dose by using all available equipment-specific dose reduction techniques.
When a PE is identified, it is characterized as acute or chronic. An embolus is acute if it is situated centrally within the vascular lumen or if it occludes a vessel (vessel cutoff sign; see the image below). Acute PE commonly causes distention of the involved vessel.
 Computed
tomography angiogram in a 53-year-old man with acute pulmonary
embolism. This image shows an intraluminal filling defect that occludes
the anterior basal segmental artery of the right lower lobe. Also
present is an infarction of the corresponding lung, which is indicated
by a triangular, pleura-based consolidation (Hampton hump). An
embolus is chronic if (1) it is eccentric and contiguous with the
vessel wall (see the image below), (2) it reduces the arterial diameter
by more than 50%, (3) evidence of recanalization within the thrombus is
present, and (4) an arterial web is present.
Computed
tomography angiogram in a 53-year-old man with acute pulmonary
embolism. This image shows an intraluminal filling defect that occludes
the anterior basal segmental artery of the right lower lobe. Also
present is an infarction of the corresponding lung, which is indicated
by a triangular, pleura-based consolidation (Hampton hump). An
embolus is chronic if (1) it is eccentric and contiguous with the
vessel wall (see the image below), (2) it reduces the arterial diameter
by more than 50%, (3) evidence of recanalization within the thrombus is
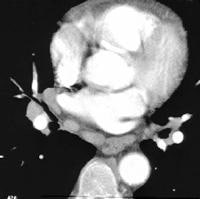
present, and (4) an arterial web is present.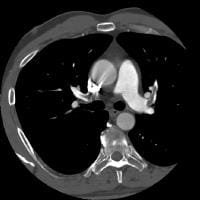 Computed
tomography angiography in a young man who experienced acute chest pain
and shortness of breath after a transcontinental flight. This image
demonstrates a clot in the anterior segmental artery in the left upper
lung (LA2) and a clot in the anterior segmental artery in the right
upper lung (RA2). A PE is further characterized as central or
peripheral, depending on the location or the arterial branch involved.
Central vascular zones include the following:
Computed
tomography angiography in a young man who experienced acute chest pain
and shortness of breath after a transcontinental flight. This image
demonstrates a clot in the anterior segmental artery in the left upper
lung (LA2) and a clot in the anterior segmental artery in the right
upper lung (RA2). A PE is further characterized as central or
peripheral, depending on the location or the arterial branch involved.
Central vascular zones include the following:main pulmonary artery
- The left and right main pulmonary arteries
- The anterior trunk
- The right and left interlobar arteries
- The left upper lobe trunk
- The right middle lobe artery
- The right and left lower lobe arteries
- The segmental and subsegmental arteries of the right upper lobe
- The right middle lobe
- The right lower lobe
- The left upper lobe
- The lingula
- The left lower lobe
Degree of confidence
In most cases, when spiral CT scan findings are positive for PE, the emboli are multiple, with intraluminal filling defects observed in the larger central arteries and in the segmental and subsegmental vessels.[19] An apparent filling defect in a single segmental or (especially) subsegmental vessel can be challenging. One should consider all the pitfalls, especially those related to volume-averaging artifacts before diagnosing an isolated subsegmental embolus. The emboli are often bilateral and more common in the arteries to the lower lobes.The sensitivity of spiral CT scanning in the evaluation of central PE is as high as 100%. However, it is reportedly variable and lower (see the table below). Also, the reported incidence of isolated subsegmental PEs varies from 5% in the Prospective Investigation of Pulmonary Embolism Diagnosis (PIOPED) study to 36% in another study.[6] Moreover, the true significance of small emboli has not been proven conclusively. Small thromboemboli may have clinical significance in patients with limited cardiopulmonary reserve.
Pulmonary angiography demonstrates subsegmental vessels in more detail than does CT scanning, although the superimposition of the small vessels remains a limiting factor. As a result, the interobserver agreement rate for isolated subsegmental PE is only 45%.[20]
Investigators have reported uneventful clinical outcomes in patients (with a negative predictive value of 99%) in whom CT scans were interpreted as negative for PE and who were not treated with anticoagulation or catheter-directed pharmacologic thrombolysis. The outcome was similar to those of patients with clinically suspected PE but without emboli on pulmonary arteriograms. This finding indicates that, although some small emboli may be missed at helical CT scanning, the subsequent morbidity rate with PE does not appear to be high.
The new MDCT scanners are considerably faster, allowing the performance of thin-section (1.25-mm) helical CT pulmonary angiography during a shorter breath hold (15-17 seconds). The segmental and subsegmental vessels are better demonstrated, findings are easier to interpret, and interobserver agreement is improved with this technique.
Although MDCT increases diagnostic capabilities, however, the large amount of data (a thin-section 16-detector row CT pulmonary angiography results in 500-600 axial slices) generated puts a substantial strain on any image analysis and archiving system. Development of dedicated algorithms for computer-aided detection and greater use of maximum intensity projection reconstruction techniques may be helpful in the future for identification of pulmonary emboli in large-volume MDCT data sets.
Table. Accuracy of helical CT* pulmonary angiography (Open Table in a new window)
| Reference | No. of Patients | Sensitivity, % | Specificity, % | Collimation and Anatomic level |
| Remy-Jardin et al, 1992[21] | 42 | 100 | 96 | 5 mm, segmental |
| Goodman et al, 1995[22] | 20 | 86 | 92 | 5 mm, segmental |
| Remy-Jardin et al, 1996[15] | 75 | 91 | 78 | 3 and 5 mm, segmental |
| Mayo et al, 1997[23] | 142 | 87 | 95 | 3 mm, segmental |
| Garg et al, 1998[24] | 54 | 67 | 100 | 3 mm, subsegmental |
| Drucker et al, 1998[25] | 47 | 53-60 | 81-97 | 5 mm, segmental |
| *Single-slice CT scanners. The accuracy with newer MDCT scanners is reported to be higher. | ||||
 Computed
tomography angiogram in a 55-year-old man with possible pulmonary
embolism. This image was obtained at the level of the lower lobes and
shows perivascular segmental enlarged lymph nodes as well as prominent
extraluminal soft tissue interposed between the artery and the bronchus.
Flow-related and motion artifacts can result in pseudofilling
defects and should be kept in mind when the quality of study is
evaluated and when the image is interpreted. Flow-related pseudofilling
defects can also result in false-positive findings on the CT venogram.
Computed
tomography angiogram in a 55-year-old man with possible pulmonary
embolism. This image was obtained at the level of the lower lobes and
shows perivascular segmental enlarged lymph nodes as well as prominent
extraluminal soft tissue interposed between the artery and the bronchus.
Flow-related and motion artifacts can result in pseudofilling
defects and should be kept in mind when the quality of study is
evaluated and when the image is interpreted. Flow-related pseudofilling
defects can also result in false-positive findings on the CT venogram. Overall, findings in 2-4% of CT pulmonary angiographic examinations are nondiagnostic because of severe motion artifacts (severe dyspnea) or poor venous access.[26] In 8-10% of examinations, the scans are suboptimal in quality; these allow for confident evaluation of only the central pulmonary arteries. In addition to CT pulmonary angiograms, CT venograms obtained may be useful in patients with a nondiagnostic angiogram, particularly if it is positive for DVT. (See the image below.)
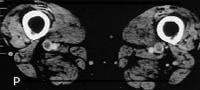 Computed
tomography venograms in a 65-year-old man with possible pulmonary
embolism. This image shows acute deep venous thrombosis with
intraluminal filling defects in the bilateral superficial femoral veins.
Computed
tomography venograms in a 65-year-old man with possible pulmonary
embolism. This image shows acute deep venous thrombosis with
intraluminal filling defects in the bilateral superficial femoral veins.
No comments:
Post a Comment