Overview
Evaluation
of the brachial plexus is a clinical challenge. Physical examination
has traditionally been a mainstay in evaluating and localizing pathology
involving the brachial plexus. Physical examination is especially
difficult in patients with scarring and fibrosis secondary to surgery or
irradiation. Electrophysiologic studies can be used to detect
abnormalities in nerve conduction, but they are poor for localizing a
lesion.[1, 2] (See the diagram below.)
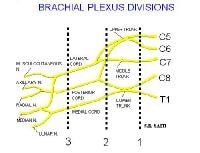 Diagram of the brachial plexus. Injury
to the brachial plexus is associated with weakness and paresthesias of
the upper extremity on the affected side. Thorough neurologic
examination can be performed to localize the injury and to help the
radiologist pinpoint the location of pathology.
Diagram of the brachial plexus. Injury
to the brachial plexus is associated with weakness and paresthesias of
the upper extremity on the affected side. Thorough neurologic
examination can be performed to localize the injury and to help the
radiologist pinpoint the location of pathology.
As the technology and resolution have improved, magnetic resonance imaging (MRI) has become increasingly important in the evaluation of brachial plexus pathology. Correlation of imaging results with electrophysiologic findings increases overall specificity and sensitivity.[3, 4, 5]
According to Nardin et al,[2, 6] electromyelography (EMG) and MRI examinations are complementary. Their study demonstrated that the sensitivity of EMG and MRI were 72% and 60%, respectively. Plain radiography can depict large lesions affecting the brachial plexus. However, radiographs are far less sensitive than other studies. Computed tomography (CT) scanning has increased sensitivity for depicting extrinsic masses that compress the nerves; however, it offers poor soft tissue contrast for direct evaluation of the nerves.
With the advent of MRI, nerves that compose the brachial plexus can now be directly evaluated. Intrinsic and extrinsic pathology can be evaluated. Exact anatomic components of the brachial plexus, such as the roots, trunks, divisions, and cords, can be identified. MRI has the additional benefit of multiplanar imaging and increased soft tissue contrast. The tissue resolution of MRI is constantly improving with new pulse sequences and coil designs.[1, 6, 7, 8, 9, 10, 11] (See the images below.)
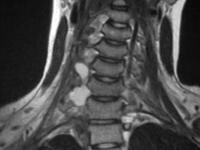
 Birth
trauma. Sagittal image of the brachial plexus shows an area of
increased signal intensity in the C6 neural foramen. This is an area of
particular concern in cases of birth trauma, and the finding is
consistent with traumatic injury of the nerve root.
Birth
trauma. Sagittal image of the brachial plexus shows an area of
increased signal intensity in the C6 neural foramen. This is an area of
particular concern in cases of birth trauma, and the finding is
consistent with traumatic injury of the nerve root. 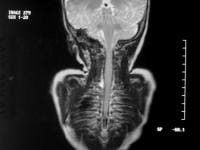 Birth trauma. Coronal image of the brachial plexus shows an area of increased signal intensity in the right C6 neural foramen.
Birth trauma. Coronal image of the brachial plexus shows an area of increased signal intensity in the right C6 neural foramen.  Birth trauma. With radiography and CT scanning, changes in the shape or position of the brachial plexus have been used to assess pathology.[12] With
MRI, the nerve can be directly visualized and evaluated for pathology.
MRI sequences such as fat-saturated T2-weighted spin-echo, short-tau
inversion recovery (STIR), and gadolinium-enhanced T1-weighted spin-echo
sequences help in depicting subtle changes in the signal intensity of
the nerves or enhancement and aid in refining the differential
diagnosis. In addition, maximum intensity projections can make
localization and visualization of the pathology most understandable for
referring clinicians and surgeons. (See the images below.)
Birth trauma. With radiography and CT scanning, changes in the shape or position of the brachial plexus have been used to assess pathology.[12] With
MRI, the nerve can be directly visualized and evaluated for pathology.
MRI sequences such as fat-saturated T2-weighted spin-echo, short-tau
inversion recovery (STIR), and gadolinium-enhanced T1-weighted spin-echo
sequences help in depicting subtle changes in the signal intensity of
the nerves or enhancement and aid in refining the differential
diagnosis. In addition, maximum intensity projections can make
localization and visualization of the pathology most understandable for
referring clinicians and surgeons. (See the images below.)
 Avulsion
in a 17-year-old female adolescent after she was ejected from an
automobile in a collision. Oblique cervical myelogram shows
extravasation of contrast material from torn right lower nerve-root
sheaths.
Avulsion
in a 17-year-old female adolescent after she was ejected from an
automobile in a collision. Oblique cervical myelogram shows
extravasation of contrast material from torn right lower nerve-root
sheaths. 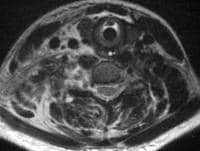 Avulsion
in a 17-year-old female adolescent after she was ejected from an
automobile in a collision. Axial image obtained with a long repetition
time (TR) and a long echo time (TE) (TR/TE, 3800/98 ms) shows extensive
injuries to the right paraspinal soft tissues. The 3 images immediately
following this one were obtained 3 months after this image was produced.
Avulsion
in a 17-year-old female adolescent after she was ejected from an
automobile in a collision. Axial image obtained with a long repetition
time (TR) and a long echo time (TE) (TR/TE, 3800/98 ms) shows extensive
injuries to the right paraspinal soft tissues. The 3 images immediately
following this one were obtained 3 months after this image was produced.
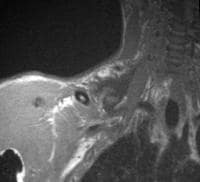
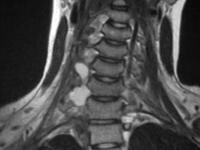 Avulsion
in a 17-year-old female adolescent after she was ejected from an
automobile in a collision. Coronal image obtained with a long repetition
time (TR) and long echo time (TE) (TR/TE, 1800/71 ms) shows
circumscribed right paravertebral fluid collections at C6-7 and C7-T1.
These represent pseudomeningoceles from torn nerve-root sheaths and
avulsed nerve roots.
Avulsion
in a 17-year-old female adolescent after she was ejected from an
automobile in a collision. Coronal image obtained with a long repetition
time (TR) and long echo time (TE) (TR/TE, 1800/71 ms) shows
circumscribed right paravertebral fluid collections at C6-7 and C7-T1.
These represent pseudomeningoceles from torn nerve-root sheaths and
avulsed nerve roots.  Avulsion
in a 17-year-old female adolescent after she was ejected from an
automobile in a collision. Sagittal image obtained with a long
repetition time (TR) and long echo time (TE) (TR/TE, 1800/112 ms) shows
circumscribed right paravertebral fluid collections at C6-7 and C7-T1.
These represent pseudomeningoceles from torn nerve-root sheaths and
avulsed nerve roots.
Avulsion
in a 17-year-old female adolescent after she was ejected from an
automobile in a collision. Sagittal image obtained with a long
repetition time (TR) and long echo time (TE) (TR/TE, 1800/112 ms) shows
circumscribed right paravertebral fluid collections at C6-7 and C7-T1.
These represent pseudomeningoceles from torn nerve-root sheaths and
avulsed nerve roots. 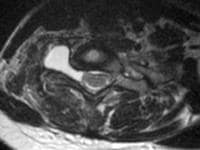 Avulsion
in a 17-year-old female adolescent after she was ejected from an
automobile in a collision. Axial image obtained with a long repetition
time (TR) and long echo time TE (TR/TE, 4000/100 ms) shows circumscribed
right paravertebral fluid collections at C6-7 and C7-T1. These
represent pseudomeningoceles from torn nerve root sheaths and avulsed
nerve roots. Gadolinium-based contrast agents (gadopentetate
dimeglumine [Magnevist], gadobenate dimeglumine [MultiHance],
gadodiamide [Omniscan], gadoversetamide [OptiMARK], gadoteridol
[ProHance]) have been linked to the development of nephrogenic systemic
fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). For more
information, see the eMedicine topic Nephrogenic Systemic Fibrosis.
The disease has occurred in patients with moderate to end-stage renal
disease after being given a gadolinium-based contrast agent to enhance
MRI or MRA scans.
Avulsion
in a 17-year-old female adolescent after she was ejected from an
automobile in a collision. Axial image obtained with a long repetition
time (TR) and long echo time TE (TR/TE, 4000/100 ms) shows circumscribed
right paravertebral fluid collections at C6-7 and C7-T1. These
represent pseudomeningoceles from torn nerve root sheaths and avulsed
nerve roots. Gadolinium-based contrast agents (gadopentetate
dimeglumine [Magnevist], gadobenate dimeglumine [MultiHance],
gadodiamide [Omniscan], gadoversetamide [OptiMARK], gadoteridol
[ProHance]) have been linked to the development of nephrogenic systemic
fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). For more
information, see the eMedicine topic Nephrogenic Systemic Fibrosis.
The disease has occurred in patients with moderate to end-stage renal
disease after being given a gadolinium-based contrast agent to enhance
MRI or MRA scans.
NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness. For more information, see Medscape.
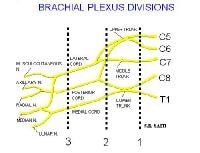 Diagram of the brachial plexus. Injury
to the brachial plexus is associated with weakness and paresthesias of
the upper extremity on the affected side. Thorough neurologic
examination can be performed to localize the injury and to help the
radiologist pinpoint the location of pathology.
Diagram of the brachial plexus. Injury
to the brachial plexus is associated with weakness and paresthesias of
the upper extremity on the affected side. Thorough neurologic
examination can be performed to localize the injury and to help the
radiologist pinpoint the location of pathology.As the technology and resolution have improved, magnetic resonance imaging (MRI) has become increasingly important in the evaluation of brachial plexus pathology. Correlation of imaging results with electrophysiologic findings increases overall specificity and sensitivity.[3, 4, 5]
According to Nardin et al,[2, 6] electromyelography (EMG) and MRI examinations are complementary. Their study demonstrated that the sensitivity of EMG and MRI were 72% and 60%, respectively. Plain radiography can depict large lesions affecting the brachial plexus. However, radiographs are far less sensitive than other studies. Computed tomography (CT) scanning has increased sensitivity for depicting extrinsic masses that compress the nerves; however, it offers poor soft tissue contrast for direct evaluation of the nerves.
With the advent of MRI, nerves that compose the brachial plexus can now be directly evaluated. Intrinsic and extrinsic pathology can be evaluated. Exact anatomic components of the brachial plexus, such as the roots, trunks, divisions, and cords, can be identified. MRI has the additional benefit of multiplanar imaging and increased soft tissue contrast. The tissue resolution of MRI is constantly improving with new pulse sequences and coil designs.[1, 6, 7, 8, 9, 10, 11] (See the images below.)
 Birth
trauma. Sagittal image of the brachial plexus shows an area of
increased signal intensity in the C6 neural foramen. This is an area of
particular concern in cases of birth trauma, and the finding is
consistent with traumatic injury of the nerve root.
Birth
trauma. Sagittal image of the brachial plexus shows an area of
increased signal intensity in the C6 neural foramen. This is an area of
particular concern in cases of birth trauma, and the finding is
consistent with traumatic injury of the nerve root. 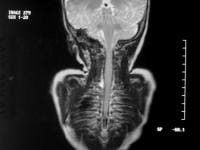 Birth trauma. Coronal image of the brachial plexus shows an area of increased signal intensity in the right C6 neural foramen.
Birth trauma. Coronal image of the brachial plexus shows an area of increased signal intensity in the right C6 neural foramen.  Birth trauma. With radiography and CT scanning, changes in the shape or position of the brachial plexus have been used to assess pathology.[12] With
MRI, the nerve can be directly visualized and evaluated for pathology.
MRI sequences such as fat-saturated T2-weighted spin-echo, short-tau
inversion recovery (STIR), and gadolinium-enhanced T1-weighted spin-echo
sequences help in depicting subtle changes in the signal intensity of
the nerves or enhancement and aid in refining the differential
diagnosis. In addition, maximum intensity projections can make
localization and visualization of the pathology most understandable for
referring clinicians and surgeons. (See the images below.)
Birth trauma. With radiography and CT scanning, changes in the shape or position of the brachial plexus have been used to assess pathology.[12] With
MRI, the nerve can be directly visualized and evaluated for pathology.
MRI sequences such as fat-saturated T2-weighted spin-echo, short-tau
inversion recovery (STIR), and gadolinium-enhanced T1-weighted spin-echo
sequences help in depicting subtle changes in the signal intensity of
the nerves or enhancement and aid in refining the differential
diagnosis. In addition, maximum intensity projections can make
localization and visualization of the pathology most understandable for
referring clinicians and surgeons. (See the images below.) Avulsion
in a 17-year-old female adolescent after she was ejected from an
automobile in a collision. Oblique cervical myelogram shows
extravasation of contrast material from torn right lower nerve-root
sheaths.
Avulsion
in a 17-year-old female adolescent after she was ejected from an
automobile in a collision. Oblique cervical myelogram shows
extravasation of contrast material from torn right lower nerve-root
sheaths. 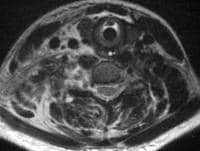 Avulsion
in a 17-year-old female adolescent after she was ejected from an
automobile in a collision. Axial image obtained with a long repetition
time (TR) and a long echo time (TE) (TR/TE, 3800/98 ms) shows extensive
injuries to the right paraspinal soft tissues. The 3 images immediately
following this one were obtained 3 months after this image was produced.
Avulsion
in a 17-year-old female adolescent after she was ejected from an
automobile in a collision. Axial image obtained with a long repetition
time (TR) and a long echo time (TE) (TR/TE, 3800/98 ms) shows extensive
injuries to the right paraspinal soft tissues. The 3 images immediately
following this one were obtained 3 months after this image was produced.
 Avulsion
in a 17-year-old female adolescent after she was ejected from an
automobile in a collision. Coronal image obtained with a long repetition
time (TR) and long echo time (TE) (TR/TE, 1800/71 ms) shows
circumscribed right paravertebral fluid collections at C6-7 and C7-T1.
These represent pseudomeningoceles from torn nerve-root sheaths and
avulsed nerve roots.
Avulsion
in a 17-year-old female adolescent after she was ejected from an
automobile in a collision. Coronal image obtained with a long repetition
time (TR) and long echo time (TE) (TR/TE, 1800/71 ms) shows
circumscribed right paravertebral fluid collections at C6-7 and C7-T1.
These represent pseudomeningoceles from torn nerve-root sheaths and
avulsed nerve roots.  Avulsion
in a 17-year-old female adolescent after she was ejected from an
automobile in a collision. Sagittal image obtained with a long
repetition time (TR) and long echo time (TE) (TR/TE, 1800/112 ms) shows
circumscribed right paravertebral fluid collections at C6-7 and C7-T1.
These represent pseudomeningoceles from torn nerve-root sheaths and
avulsed nerve roots.
Avulsion
in a 17-year-old female adolescent after she was ejected from an
automobile in a collision. Sagittal image obtained with a long
repetition time (TR) and long echo time (TE) (TR/TE, 1800/112 ms) shows
circumscribed right paravertebral fluid collections at C6-7 and C7-T1.
These represent pseudomeningoceles from torn nerve-root sheaths and
avulsed nerve roots. 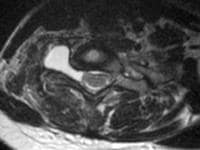 Avulsion
in a 17-year-old female adolescent after she was ejected from an
automobile in a collision. Axial image obtained with a long repetition
time (TR) and long echo time TE (TR/TE, 4000/100 ms) shows circumscribed
right paravertebral fluid collections at C6-7 and C7-T1. These
represent pseudomeningoceles from torn nerve root sheaths and avulsed
nerve roots. Gadolinium-based contrast agents (gadopentetate
dimeglumine [Magnevist], gadobenate dimeglumine [MultiHance],
gadodiamide [Omniscan], gadoversetamide [OptiMARK], gadoteridol
[ProHance]) have been linked to the development of nephrogenic systemic
fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). For more
information, see the eMedicine topic Nephrogenic Systemic Fibrosis.
The disease has occurred in patients with moderate to end-stage renal
disease after being given a gadolinium-based contrast agent to enhance
MRI or MRA scans.
Avulsion
in a 17-year-old female adolescent after she was ejected from an
automobile in a collision. Axial image obtained with a long repetition
time (TR) and long echo time TE (TR/TE, 4000/100 ms) shows circumscribed
right paravertebral fluid collections at C6-7 and C7-T1. These
represent pseudomeningoceles from torn nerve root sheaths and avulsed
nerve roots. Gadolinium-based contrast agents (gadopentetate
dimeglumine [Magnevist], gadobenate dimeglumine [MultiHance],
gadodiamide [Omniscan], gadoversetamide [OptiMARK], gadoteridol
[ProHance]) have been linked to the development of nephrogenic systemic
fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). For more
information, see the eMedicine topic Nephrogenic Systemic Fibrosis.
The disease has occurred in patients with moderate to end-stage renal
disease after being given a gadolinium-based contrast agent to enhance
MRI or MRA scans.NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness. For more information, see Medscape.
Technique and Imaging Parameters
The brachial plexus can be easily identified on MRI by first identifying the anterior scalene muscle. The brachial plexus and subclavian artery (relationship outlined above) are deep to the anterior scalene. Normal components of the brachial plexus have low signal intensity on images obtained with all sequences and are surrounded by fat. The roots are best seen on axial images, whereas the remaining components are well seen on coronal and sagittal images.[7, 13, 14] (See the images below.)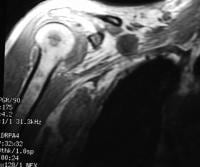 Non-Hodgkin
lymphoma in a 58-year-old man. Coronal spoiled gradient-echo image
(repetition time [TR]/echo time [TE], 175/4.2 ms; flip angle, 90°) shows
lymphomatous lesions in the right brachial plexus and in the marrow of
the humerus.
Non-Hodgkin
lymphoma in a 58-year-old man. Coronal spoiled gradient-echo image
(repetition time [TR]/echo time [TE], 175/4.2 ms; flip angle, 90°) shows
lymphomatous lesions in the right brachial plexus and in the marrow of
the humerus. 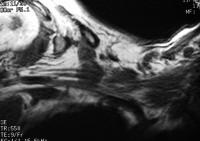 Non-Hodgkin
lymphoma. Axial image obtained with a short repetition time (TR) and
short echo time (TE) (TR/TE, 550/9 ms) shows lymphomatous lesions in the
right brachial plexus and in the marrow of the humerus.
Non-Hodgkin
lymphoma. Axial image obtained with a short repetition time (TR) and
short echo time (TE) (TR/TE, 550/9 ms) shows lymphomatous lesions in the
right brachial plexus and in the marrow of the humerus. 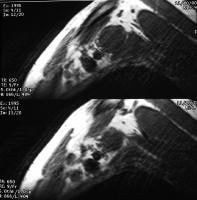 Non-Hodgkin
lymphoma in a 58-year-old man. Sagittal images obtained with a short
repetition time (TR) and a short echo time (TE) (TR/TE, 650/9 ms) show
lymphomatous lesions in the right brachial plexus and in the marrow of
the humerus.
Non-Hodgkin
lymphoma in a 58-year-old man. Sagittal images obtained with a short
repetition time (TR) and a short echo time (TE) (TR/TE, 650/9 ms) show
lymphomatous lesions in the right brachial plexus and in the marrow of
the humerus. Radiofrequency coil
A surface coil provides resolution higher than that of a body coil, but it increases artifact due to respiratory motion. A combination of each may be used in sequences for the brachial plexus. As such, the surface coil is used for the spinal cord and exiting spinal nerve roots, whereas the body coil is used to image the plexus lateral to the interscalene triangle.Field of view
Examination of the brachial plexus begins with the roots and trucks in the proximal aspects within the supraclavicular region and continues to the origin of the terminal branches at the lateral margin of the pectoralis minor muscle in the infraclavicular region.The field of view (FOV) is 17-22 cm for the direct coronal orientation and 14-17 cm for sagittal or oblique sagittal orientations.
Matrix
A matrix of 512 X 256 or 512 X 512 is used.Section thickness
The recommended section thickness is 4 mm with an intersection gap of 0-0.5 mm for direct coronal imaging and 4 mm with an intersection gap of 1-2 mm for sagittal or oblique sagittal imaging. If axial images are obtained, 4-mm thickness with a 1- to 1.5-mm intersection gap may be performed.Orientation
Images should be obtained in 2 planes. Direct coronal plane imaging is preferred over oblique coronal imaging because the brachial plexus has a shallow obliquity relative to the true coronal plane and because it can be imaged on 1 or 2 coronal sections.Cross-sectional imaging of the nerve components of the plexus may be performed by using either the true sagittal or the oblique sagittal plane on the side of interest. True sagittal imaging allows for comparison with the standard cross-sectional anatomy, which some find helpful in the recognition of appropriate anatomic landmarks. However, oblique sagittal imaging represents the true cross-section of the plexus more accurately than true sagittal imaging and thus allows for increased sensitivity to pathology, including changes in caliber, alteration in signal intensity, or presence of a fascicular pattern to the nerve components.
Some institutions include a contrast-enhanced T1-weighted axial sequence as part of their routine evaluation of the brachial plexus.
 Avulsion
in a 15-year-old male adolescent with palsy of the right upper
extremity due to trauma related to a snowmobile accident. Coronal image
obtain with a short repetition time (TR) and a short echo time (TE)
(TR/TE, 600/8 ms) shows a poorly defined zone of low signal intensity in
the region of the right brachial plexus.
Avulsion
in a 15-year-old male adolescent with palsy of the right upper
extremity due to trauma related to a snowmobile accident. Coronal image
obtain with a short repetition time (TR) and a short echo time (TE)
(TR/TE, 600/8 ms) shows a poorly defined zone of low signal intensity in
the region of the right brachial plexus.  Avulsion
in a 15-year-old male adolescent with palsy of the right upper
extremity due to trauma related to a snowmobile accident. Coronal image
obtained with a long repetition time (TR) and a long echo time (TE)
(TR/TE, 7058/98 ms) shows a traumatic fluid collection containing
several retracted nerves of the right brachial plexus.
Avulsion
in a 15-year-old male adolescent with palsy of the right upper
extremity due to trauma related to a snowmobile accident. Coronal image
obtained with a long repetition time (TR) and a long echo time (TE)
(TR/TE, 7058/98 ms) shows a traumatic fluid collection containing
several retracted nerves of the right brachial plexus. 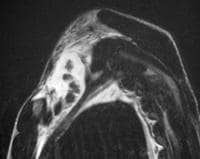 Avulsion
in a 15-year-old male adolescent with palsy of the right upper
extremity due to trauma related to a snowmobile accident. Sagittal image
obtained a long repetition time (TR) and long echo time (TE) (TR/TE,
10,588/98 ms) shows a traumatic fluid collection containing several
retracted nerves of the right brachial plexus.
Avulsion
in a 15-year-old male adolescent with palsy of the right upper
extremity due to trauma related to a snowmobile accident. Sagittal image
obtained a long repetition time (TR) and long echo time (TE) (TR/TE,
10,588/98 ms) shows a traumatic fluid collection containing several
retracted nerves of the right brachial plexus. 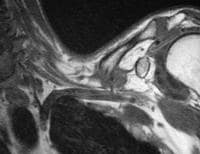 Clavicular
fracture in a 57-year-old man with a traumatic comminuted fracture of
the left clavicle. Coronal image obtained with a short repetition time
(TR) and a short echo time (TE) (TR/TE, 600/9 ms) shows the fracture
mildly impressing on the left brachial plexus.
Clavicular
fracture in a 57-year-old man with a traumatic comminuted fracture of
the left clavicle. Coronal image obtained with a short repetition time
(TR) and a short echo time (TE) (TR/TE, 600/9 ms) shows the fracture
mildly impressing on the left brachial plexus. 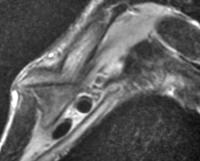 Clavicular
fracture in a 57-year-old man with a traumatic comminuted fracture of
the left clavicle. Sagittal image obtained with a long repetition time
(TR) and long echo time (TE) (TR/TE, 2000/83 ms) shows the fracture
mildly impressing on the left brachial plexus.
Clavicular
fracture in a 57-year-old man with a traumatic comminuted fracture of
the left clavicle. Sagittal image obtained with a long repetition time
(TR) and long echo time (TE) (TR/TE, 2000/83 ms) shows the fracture
mildly impressing on the left brachial plexus. 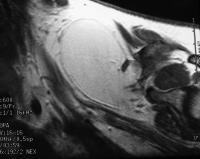 Lipoma
in a 38-year-old woman with a lipoma above the left brachial plexus.
Coronal image obtained with a short repetition time (TR) and short echo
time (TE) (TR/TE, 600/9 ms) shows a lipoma mildly impressing on the left
brachial plexus.
Lipoma
in a 38-year-old woman with a lipoma above the left brachial plexus.
Coronal image obtained with a short repetition time (TR) and short echo
time (TE) (TR/TE, 600/9 ms) shows a lipoma mildly impressing on the left
brachial plexus. 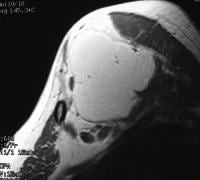 Lipoma
in a 38-year-old woman with a lipoma above the left brachial plexus.
Sagittal image obtained with a short repetition time (TR) and short echo
time (TE) (TR/TE, 600/9 ms) shows a lipoma mildly impressing on the
left brachial plexus.
Lipoma
in a 38-year-old woman with a lipoma above the left brachial plexus.
Sagittal image obtained with a short repetition time (TR) and short echo
time (TE) (TR/TE, 600/9 ms) shows a lipoma mildly impressing on the
left brachial plexus. 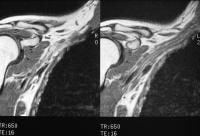 Neurofibromatosis
type 1 in a 26-year-old woman. Coronal images obtained with a short
repetition time (TR) and a short echo time (TE) (TR/TE 650/16 ms) show
several circumscribed neurofibromas along the right brachial plexus.
Neurofibromatosis
type 1 in a 26-year-old woman. Coronal images obtained with a short
repetition time (TR) and a short echo time (TE) (TR/TE 650/16 ms) show
several circumscribed neurofibromas along the right brachial plexus. 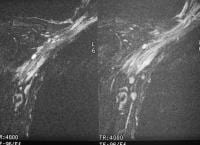 Neurofibromatosis
type 1 in a 26-year-old woman. Coronal fat-suppressed images obtained
with a long repetition time (TR) and a long echo time (TE) (TR/TE,
4000/96 ms) show several circumscribed neurofibromas along the right
brachial plexus. The neurofibromas have high signal intensity.
Neurofibromatosis
type 1 in a 26-year-old woman. Coronal fat-suppressed images obtained
with a long repetition time (TR) and a long echo time (TE) (TR/TE,
4000/96 ms) show several circumscribed neurofibromas along the right
brachial plexus. The neurofibromas have high signal intensity. 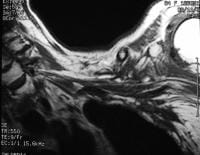 Postirradiation
changes in an 84-year-old woman with a history of breast cancer.
Coronal image obtained with a short repetition time (TR) and short echo
time (TE) (TR/TE, 400/9 ms) shows irregular thickening of the left
brachial plexus.
Postirradiation
changes in an 84-year-old woman with a history of breast cancer.
Coronal image obtained with a short repetition time (TR) and short echo
time (TE) (TR/TE, 400/9 ms) shows irregular thickening of the left
brachial plexus.  Postirradiation
changes in an 84-year-old with a history of breast cancer. Coronal
contrast-enhanced fat-suppressed image obtained with a short repetition
time (TR) and a short echo time (TE) (TR/TE, 650/9 ms) shows poorly
defined zones of contrast enhancement in the region of the brachial
plexus. These zones representing radiation-induced changes to
infiltrating tumor.
Postirradiation
changes in an 84-year-old with a history of breast cancer. Coronal
contrast-enhanced fat-suppressed image obtained with a short repetition
time (TR) and a short echo time (TE) (TR/TE, 650/9 ms) shows poorly
defined zones of contrast enhancement in the region of the brachial
plexus. These zones representing radiation-induced changes to
infiltrating tumor. Pulse sequences
T1- and T2-weighted images are obtained with identical parameters in terms of FOV, matrix, section thickness, and imaging plane.STIR or frequency-selective fat-saturation methods may be used for T2-weighted MRI to increase the conspicuity of abnormal signal intensity from the signal intensity of adjacent fat. Each has its advantages and disadvantages. STIR has been described as being more reliable than the other method because of its uniform and consistent fat suppression and excellent T2-like contrast when long repetition times are used.
The STIR method has several disadvantages. For example, it has a relatively low signal-to-noise ratio, it offers relatively low tissue contrast, and it is more susceptible to flow artifacts than other methods.
In contrast, frequency-selective fat-saturation methods have the advantage of an improved signal-to-noise ratio, T1-weighted imaging, and reduced flow-related artifacts. The major disadvantage of this type of fat suppression is the nonuniformity of fat suppression with the FOV primarily from inhomogeneity of B0. This variability in fat suppression is exacerbated by the nonuniformity in B1.
When radiation injury, neoplasm, infection, or inflammatory etiologies are present or suspected, contrast-enhanced fat-suppressed T1-weighted MRI should be performed. The suggested protocol is summarized in in the image below.
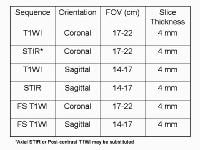 Summary
of suggested MRI techniques. FOV = field of view; T1WI = T1-weighted
imaging; STIR = short-tau inversion recovery; FS = fast spin echo.
Summary
of suggested MRI techniques. FOV = field of view; T1WI = T1-weighted
imaging; STIR = short-tau inversion recovery; FS = fast spin echo.
I was diagnosed of Herpes 2years ago and I have tried all possible means to get the cure but all to no avail, until i saw a post in a health forum about a Herbal Doctor(Dr imoloa who prepares herbal medicine to cure all kind of diseases including Herpes, at first i doubted, if it was real but decided to give him a trial, when i contacted Dr imoloa through his Email: drimolaherbalmademedicine@gmail.com he guided me and prepared a herbal medicine and sent it to me via courier Delivery service,when i received the package (herbal medicine) He gave me instructions on how to consume it, i started using it as instructed and i stop getting outbreaks and the sores started vanishing, could you believe i was cured of this deadly virus within two to three weeks and notices changes in my body. Days of using this REMEDY,couldn't believe the healing at first until i see it as my HERPES get cleared like magic Dr imoloa also use his herbal medicine to cure diseases like, HIV/aids, lupus disease, dry cough, fever, malaria, bronchitis disease, cystic fibrosis, Lyme disease, acute myeloid leukaemia, alzheimer's disease, blood poisoning, measles, kidney cancer, kidney infections, diarrhoea, epilepsy, joint pain, mouth ulcer,bowel cancer, discoid eczema, eye cancer, food poisoning, fibroid, hairy cell leukaemia, mouth cancer, skin disease, lung cancer, rheumatoid lung disease, liver disease, penile cancer, parkinson disease, arthritis, breast cancer, bone cancer hepatitis A.B.C, Diabetes, fatigue, muscle aches, anal cancer, asthma, Contact this great herbal Doctor today the father of herbalism. via Email: drimolaherbalmademedicine@gmail.com or whatssapp him +2347081986098. and get cured permanently He is real..
ReplyDelete